Transporters and Drug-Metabolizing Enzymes in Drug Toxicity » książka



Transporters and Drug-Metabolizing Enzymes in Drug Toxicity
ISBN-13: 9781119170846 / Angielski / Twarda / 2021 / 528 str.
Transporters and Drug-Metabolizing Enzymes in Drug Toxicity
ISBN-13: 9781119170846 / Angielski / Twarda / 2021 / 528 str.
(netto: 878,64 VAT: 5%)
Najniższa cena z 30 dni: 911,31
ok. 30 dni roboczych.
Darmowa dostawa!
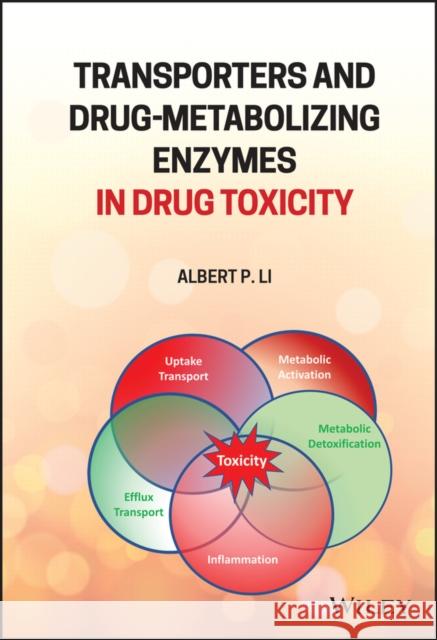
Accurate assessment of human drug toxicity is a major challenge in the pharmaceutical industry. Drug metabolism and toxicology are two scientific disciplines that traditionally have been considered independently. For instance, in drug development, drug candidates are evaluated for properties in these two disciplines in different departments. It is now becoming apparent that the two disciplines are closely related in terms of safety evaluation. Transporters and Drug-Metabolizing Enzymes in Drug Toxicity provides a comprehensive and up-to-date coverage of the relationship between drug metabolism enzymes and transporters on drug toxicity. It brings together the scientific disciplines of drug metabolism and toxicology, with a focus on the role of biotransformation on drug toxicity and as a major factor for species and individual differences. In addition, the author describes promising experimental approaches to accurately assess human drug toxicity via the incorporation of human-specific drug metabolism in toxicity assays. Offering a valuable resource for those scientific professionals and researchers involved with drug development, pharmacology, and toxicology; Transporters and Drug-Metabolizing Enzymes in Drug Toxicity features key benefits that include: - Unites both the metabolism and transporter components of drug toxicity - two aspects not normally connected and the latter often neglected - Familiarizes readers with the mechanism and species differences in drug metabolizing enzymes and transporters - Describes methods to investigate the role drug metabolizing enzymes and transporters in drug toxicity
This book provides a comprehensive and up–to–date coverage of the relationship between drug metabolism enzymes and transporters on drug toxicity.
Preface xixList of Contributors xxiPart I Overview 11 Overview: Drug Metabolism, Transporter-Mediated Uptake and Efflux, and Drug Toxicity 3Albert P. Li1.1 Drug Toxicity as a Challenge in Drug Development 31.2 Fate of an Orally Administered Drug 41.3 The Multiple Determinant Hypothesis for Idiosyncratic Drug Toxicity 51.4 Concluding Remarks 71.4.1 A Comprehensive Approach to Safety Evaluation in Drug Development 71.4.2 The Dose Makes the Poison - Paracelsus Updated 8References 82 Transporter, Drug Metabolism, and Drug-Induced Liver Injury in Marketed Drugs 11Minjun Chen, Kristin Ashby, and Yue Wu2.1 Introduction 112.2 Hepatic Metabolism 122.2.1 Phase I Metabolism 122.2.2 Phase II Metabolism 142.3 Reactive Metabolite Formation and Assessment 142.3.1 Metabolism and Reactive Metabolites 152.3.2 Dose and Reactive Mtabolites 162.3.3 Structural Alerts for Avoiding Reactive Metabolites 162.3.4 Experimental Approaches for Assessing Reactive Metabolites 182.3.4.1 Covalent Binding Assay 182.3.4.2 Electrophile Trapping Experiments 182.3.4.3 Time Dependent Inactivation of CYP450 Enzymes 192.4 Hepatic Transporters 202.5 Genetic Variants and Their Impact for Pharmacokinetic Behavior and Safety 242.5.1 CYP3A4242.5.2 CYP3A5262.5.3 CYP2D6262.5.4 CYP2C9272.5.5 CYP2C19272.5.6 CYP2B6282.5.7 UGT1A1282.5.8 NAT2 282.5.9 Hepatic Transporters 292.6 Summary 29Acknowledgment 30Disclaimer 30References 303 Drug-Metabolism Enzymes and Transporter Activities as Risk Factors of Selected Marketed Drugs Associated with Drug-Induced Fatalities 41Albert P. Li3.1 Introduction 413.2 Acetaminophen 413.2.1 Drug Metabolism and Toxicity 423.2.2 Transporters and Toxicity 423.2.3 Risk Factors 433.3 Cerivastatin 433.3.1 Drug Metabolism and Toxicity 433.3.2 Transporter and Toxicity 443.3.3 Risk Factors 443.4 Felbamate 453.4.1 Drug Metabolism and Toxicity 453.4.2 Transporters and Toxicity 463.4.3 Risk Factors 463.5 Flucloxacillin 463.5.1 Drug Metabolism and Toxicity 463.5.2 Transporters and Toxicity 473.5.3 Risk Factors 473.6 Nefazodone 473.6.1 Drug Metabolism and Toxicity 483.6.2 Transporters and Toxicity 483.6.3 Risk Factors 483.7 Obeticholic Acid 493.7.1 Drug Metabolism and Toxicity 493.7.2 Transporters and Toxicity 503.7.3 Risk Factors 503.8 Sitaxentan 503.8.1 Drug Metabolism and Toxicity 513.8.2 Transporters and Toxicity 513.8.3 Risk Factors 513.9 Sorivudine 523.9.1 Drug Metabolism and Toxicity 523.9.2 Transporters and Toxicity 523.9.3 Risk Factors 523.10 Tacrine 523.10.1 Drug Metabolism and Toxicity 543.10.2 Transporters and Toxicity 543.10.3 Risk Factors 543.11 Terfenadine 553.11.1 Drug Metabolism and Toxicity 553.11.2 Transporter and Toxicity 563.11.3 Risk Factors 563.12 Troglitazone (Rezulin(r)) 563.12.1 Drug Metabolism and Toxicity 573.12.2 Transporter and Toxicity 573.12.3 Risk Factors 583.13 Trovafloxacin 583.13.1 Metabolism and Toxicity 593.13.2 Transporters and Toxicity 593.13.3 Risk Factors 593.14 Conclusions 60References 61Part II Drug Metabolizing Enzymes and Drug Toxicity 794 Drug-Metabolizing Enzymes and Drug Toxicity 81Albert P. Li4.1 Introduction 814.2 Drug-Metabolism Enzymes Involved in Metabolic Activation and Detoxification 814.3 Cytochrome P450 Monooxygenase (CYP) 824.3.1 CYP1A 824.3.1.1 Metabolic Activation 824.3.1.2 Drug Substrates 834.3.1.3 Inducers 834.3.1.4 Inhibitors 834.3.1.5 Individual Variations 834.3.1.6 Involvement in Drug Toxicity 834.3.2 CYP2A6 844.3.2.1 Substrates 844.3.2.2 Inducers 844.3.2.3 Inhibitors 844.3.2.4 Individual Variations 854.3.2.5 Involvement in Drug Toxicity 854.3.3 CYP2B6 854.3.3.1 Substrates 854.3.3.2 Inducers 864.3.3.3 Inhibitors 864.3.3.4 Individual Variations 864.3.3.5 Involvement in Drug Toxicity 864.3.4 CYP2C8 874.3.4.1 Substrates 874.3.4.2 Inducers 874.3.4.3 Inhibitors 874.3.4.4 Individual Variations 884.3.4.5 Involvement in Drug Toxicity 884.3.5 CYP2C9 884.3.5.1 Substrates 884.3.5.2 Inducers 884.3.5.3 Inhibitors 884.3.5.4 Individual Variations 894.3.5.5 Involvement in Drug Toxicity 894.3.6 CYP2C19 894.3.6.1 Substrates 894.3.6.2 Inducers 894.3.6.3 Inhibitors 894.3.6.4 Individual Variations 904.3.6.5 Involvement in Drug Toxicity 904.3.7 CYP2D6 904.3.7.1 Substrates 904.3.7.2 Inducers 904.3.7.3 Inhibitors 904.3.7.4 Individual Variations 904.3.7.5 Involvement in Drug Toxicity 914.3.8 CYP2E1 914.3.8.1 Substrates 914.3.8.2 Inducers 914.3.8.3 Inhibitors 914.3.8.4 Involvement in Drug Toxicity 914.3.9 CYP2J2 924.3.9.1 Substrates 924.3.9.2 Inhibitors 924.3.9.3 Inducers 924.3.9.4 Individual Variations 924.3.9.5 Involvement in Drug Toxicity 924.3.10 CYP3A 934.3.10.1 Substrates 934.3.10.2 Inducers 934.3.10.3 Inhibitors 934.3.10.4 Individual Variations 934.3.10.5 Involvement in Drug Toxicity 944.4 Non-P450 Drug-Metabolizing Enzymes 944.4.1 Flavin-Containing Monooxygenases (FMOs) 944.4.1.1 Substrates 944.4.1.2 Inducers 954.4.1.3 Inhibitors 954.4.1.4 Individual Variations 954.4.1.5 Involvement in Drug Toxicity 954.4.2 Monoamine Oxidase (MAO) 954.4.2.1 Substrates 964.4.2.2 Inducers 964.4.2.3 Inhibitors 964.4.2.4 Individual Variations 964.4.2.5 Involvement in Drug Toxicity 964.4.3 Alcohol Dehydrogenase (ADH) and Aldehyde Dehydrogenase (ALDH) 974.4.3.1 Substrates 974.4.3.2 Inducers 974.4.3.3 Inhibitors 974.4.3.4 Individual Variations 974.4.3.5 Involvement in Drug Toxicity 984.4.4 Aldehyde Oxidase (AOX) 984.4.4.1 Substrates 984.4.4.2 Inducers 984.4.4.3 Inhibitors 984.4.4.4 Individual Variations 994.4.4.5 Involvement in drug toxicity 994.4.5 Carboxylesterases (CESs) 994.4.5.1 Substrates 994.4.5.2 Inducers 994.4.5.3 Inhibitors 1004.4.5.4 Individual Variations 1004.4.5.5 Involvement in Drug Toxicity 1004.4.6 N-Acetyltransferase (NAT) 1004.4.6.1 Substrates 1004.4.6.2 Inducers 1004.4.6.3 Inhibitors 1014.4.6.4 Individual Variations 1014.4.6.5 Involvement in Drug Toxicity 1014.4.7 Glutathione Transferase (GST) 1014.4.7.1 Substrates 1014.4.7.2 Inducers 1024.4.7.3 Inhibitors 1024.4.7.4 Individual Variations 1024.4.7.5 Involvement in Drug Toxicity 1024.4.8 Methyltransferase (MT) 1034.4.8.1 Substrates 1034.4.8.2 Inhibitors 1034.4.8.3 Individual Variations 1034.4.8.4 Involvement in Drug Toxicity 1034.4.9 Uridine Glucuronosyltransferase (UGT) 1034.4.9.1 Substrates 1044.4.9.2 Inducers 1044.4.9.3 Inhibitors 1044.4.9.4 Individual Variations 1044.4.9.5 Involvement in Drug Toxicity 1044.4.10 Sulfotransferase (SULT) 1054.4.10.1 Substrates 1054.4.10.2 Inducers 1054.4.10.3 Inhibitors 1064.4.10.4 Individual Variations 1064.4.10.5 Involvement in Drug Toxicity 1064.5 Conclusions 106References 1075 Genetic Polymorphism of Drug-Metabolizing Enzymes and Drug Transporters in Drug Toxicity 139Ann K. Daly5.1 Introduction 1395.2 Drug-Induced Liver Injury 1405.2.1 Background 1405.2.2 Polymorphisms Affecting Drug Metabolism and DILI 1405.2.2.1 Isoniazid 1405.2.2.2 Diclofenac 1465.2.2.3 Tolcapone 1465.2.2.4 Ticlopidine 1475.2.2.5 Efavirenz 1475.2.2.6 Troglitazone 1475.2.3 Polymorphisms Affecting Transporters and DILI 1475.3 Drug-Induced Skin Injury and Related Hypersensitivity Reactions 1495.4 Statin-Induced Myopathy 1515.4.1 Background 1515.4.2 Cytochromes P450 1515.4.3 Transporters 1525.5 Conclusions 154References 1546 Acyl Glucuronidation and Acyl-CoA Formation Mechanisms Mediating the Bioactivation and Potential Toxicity of Carboxylic Acid-containing Drugs 167Mark P. Grillo6.1 Introduction 1676.2 Phase II Metabolism 1716.2.1 Glucuronidation 1716.2.2 Acyl-CoA Thioester Formation 1716.3 Chemical Stability of Phase II Metabolites 1726.3.1 Acyl Glucuronide Instability 1726.3.2 Acyl-CoA Thioester Stability 1756.4 Phase II Metabolite Chemical Reactivity 1766.4.1 Acyl Glucuronide Reactivity with Nucleophiles In vitro 1766.4.2 Acyl-CoA Thioester Reactivity with Nucleophiles In vitro 1806.5 Phase II Metabolite-Mediated Covalent Binding 1836.5.1 Acyl Glucuronide-Mediated covalent Binding to protein 1836.5.2 Acyl-CoA Thioester-Mediated Covalent Binding to Protein 1856.6 Phase II Metabolite Prediction of Covalent Binding 1876.6.1 Prediction of Covalent Binding to Protein by Acyl Glucuronides 1876.6.2 Prediction of Covalent Binding to Protein by Acyl-CoA Thioesters 1896.7 Studies Directly Comparing Carboxylic Acid Drug Bioactivation by Acyl Glucuronidation and Acyl-CoA Formation 1906.8 Prediction of Drug-Induced Liver Injury for Carboxylic Acid Drugs 1946.9 Conclusions 196References 1977 Liquid Chromatography-Mass Spectrometry (LC-MS) Quantification of Reactive Metabolites 207Qingping Wang and Chuang Lu7.1 Introduction 2077.2 LC-MS Methods Using GSH as a Trapping Reagent 2097.2.1 LC-MS Approaches at Positive Mode Using Constant Neutral Loss (CNL) Scan or Enhanced Product Ion (EPI) Scan 2097.2.2 LC-MS Approaches at Negative Mode Using Neutral Loss, Pre-Ion Scan (PIS) and XoPI (Extraction of Product Ion) 2127.2.3 LC-MS Approaches Using Stable Isotopic-GSH 2137.2.4 LC-MS Approaches Using Combined XoPI and Stable-Isotopic GSH 2147.2.5 LC-MS Coupled with Software-Assisted Approach 2187.2.6 Using GSH Derivatives as Trapping Reagents for Detection and Quantitation 2197.3 Using Other Trapping Reagents 2227.4 Identification and Characterization of Rearranged GSH Adducts 2227.5 Strategies for Optimization and Decision Tree 2247.6 Summary 226Acknowledgment 227Abbreviations 227References 2288 Human-Based In Vitro Experimental Approaches for the Evaluation of Metabolism-Dependent Drug Toxicity 235Albert P. Li8.1 Introduction 2358.2 Assays for Reactive Metabolites 2358.2.1 Glutathione Trapping Assay 2368.2.2 Covalent Binding Assay 2368.3 Cell-Based Assays for Metabolism-Dependent Toxicity 2378.4 Primary Human Hepatocyte Assays for Metabolism-Dependent Drug Toxicity 2388.4.1 In Vitro Screening Assays for Hepatotoxicity 2388.4.2 Cytotoxic Metabolic Pathway Identification Assay (CMPIA) 2388.4.3 Metabolic Comparative Cytotoxicity Assay (MCCA) 2418.4.4 MetMax(TM) Cryopreserved Human Hepatocytes (MMHH) Metabolic Activation Cytotoxicity Assay (MMACA) 2428.5 Emerging Hepatocyte Technologies for the Evaluation of Drug Toxicity 2428.5.1 Human Hepatocytes ROS/ATP Assay for DILI Drugs 2428.5.2 Long-Term Hepatocyte Cultures 2448.5.2.1 999Elite(TM) Long-Term Cultured Human Hepatocytes 2448.5.2.2 Hepatocyte/Non-Hepatocyte Cocultures 2448.5.2.3 Human Hepatocyte Spheroids 2458.5.2.4 Microfluidic 3-Dimensional (3-d) Hepatocyte Cultures 2458.6 Integrated Discrete Multiple Organ Coculture (IdMOC(r)) 2478.7 Conclusion 249References 251Part III Drug Transporters and Drug Toxicity 2619 Mechanism-Based Experimental Models for the Evaluation of BSEP Inhibition and DILI 263William A. Murphy, Chitra Saran, Paavo Honkakoski, and Kim L.R. Brouwer9.1 Introduction 2639.1.1 Drug-Induced Liver Injury 2639.1.2 Bile Acid Homeostasis and Role of Bile Salt Export Pump 2649.2 Membrane Vesicles to Study BSEP Inhibition 2669.2.1 Membrane Vesicle Preparations 2679.2.2 Membrane Vesicle Assays and Data Interpretation 2689.3 Sandwich-Cultured Hepatocytes to Study BSEP Inhibition 2709.3.1 B-CLEAR(r) Assay 2709.3.2 Uptake and Efflux Studies with Mechanistic Modeling 2739.4 Other In Vitro Methods to Study BSEP Inhibition 2759.5 Computational Methods Used to Predict BSEP Inhibition 2779.6 In Vitro Models as a Predictor of Clinical DILI 2789.6.1 The C-DILI(TM) Assay 2789.7 Preclinical In Vivo Models for the Evaluation of BSEP/Bsep Inhibition and DILI 2799.8 In Vivo Clinical Biomarkers of BSEP Inhibition and DILI 2829.8.1 Serum Bile Acids as Clinical Biomarkers 2829.8.2 Clinical Biomarkers of DILI 2839.9 Quantitative Systems Toxicology to Predict DILI 2849.10 Conclusions 287Funding Information 287Conflict of Interest 288Acknowledgments 288Reference 28810 Hepatic Bile Acid Transporters in Drug-Induced Cholestasis 307Tao Hu and Hongbing WangAbbreviations 30710.1 Introduction 30810.2 Bile Acid and DIC 30810.2.1 Bile Acid 30910.2.1.1 Bile Acid Synthesis 30910.2.1.2 Bile Acid Transport 31010.2.2 Cytotoxicity of Bile Acids and DIC 31010.3 Hepatic Bile Acid Uptake Transporters in DIC 31210.3.1 Sodium-Taurocholate Cotransporting Polypeptide (NTCP) 31210.3.1.1 Substrates of NTCP 31410.3.1.2 Regulation of NTCP 31510.3.1.3 NTCP and Cholestasis 31610.3.2 Other Hepatic Bile Acid Uptake Transporters 31710.4 Hepatic Bile Acid Efflux Transporters in DIC 31710.4.1 Bile Salt Export Pump (BSEP) 31810.4.1.1 Substrates of BSEP 31810.4.1.2 Regulation of BSEP 31910.4.1.3 Internalization of BSEP 32110.4.1.4 BSEP and Cholestasis 32110.4.2 Other Hepatic Bile Acid Efflux Transporters 32310.4.2.1 MRP2 32310.4.2.2 MRP3 and MRP4 32410.5 Bidirectional Bile Acid Transporter OSTalpha/ß 32410.6 Summary 325References 32611 Role of Renal Transporters in Drug-Drug Interactions and Nephrotoxicity 339Yan Zhang and Donald Miller11.1 Overview of Renal Transporters 33911.1.1 Basolateral Transporters 34011.1.2 Apical Transporters 34111.2 Renal Transporters and Drug-Drug Interactions 34311.2.1 Impact on the Pharmacokinetics of Drugs 34411.2.2 Impact on the Drug PD 35011.3 Renal Transporters and Nephrotoxicity 35211.3.1 Nephrotoxicity Unrelated to Drug Transporters 35311.3.2 Nephrotoxicity Related to Drug Transporters 35511.4 Biomarkers and Nephrotoxicity 35911.4.1 Biomarkers for Detecting Glomerular Injury 35911.4.2 Biomarkers for Drug-Induced Injury to Proximal and Distal Tubules 36111.5 Conclusion 362References 36512 Blood-Brain Barrier Transporters and Central Nervous System Drug Response and Toxicity 377Donald W. Miller, Stacey Line, Nur A. Safa, and Yan Zhang12.1 Over-View of the Brain Barriers 37712.1.1 Blood-Brain Barrier (BBB) 37712.1.2 Blood-Cerebrospinal Fluid Barrier (BCSFB) 37912.1.3 CSF as Predictor of Drug Exposure in the Brain 37912.1.4 Solute Carriers in the BBB 38012.1.5 Drug Efflux Transporters in the BBB 38012.2 General Influence of BBB Transporters on Drug Entry into the Brain 38312.3 BBB-Transporter Effects on CNS Drug Response 38612.3.1 Influence of Efflux Transporters on Brain Disposition of Drugs 38612.3.1.1 Anticancer Agents 38612.3.1.2 Opioids 38812.3.2 SLCs and BBB Transport of Drugs 39112.4 Transporter Considerations Influencing CNS Drug Response 39112.4.1 Transporter Polymorphisms 39112.4.1.1 P-gp Polymorphism 39112.4.1.2 BCRP Polymorphism 39312.4.1.3 SLC Polymorphism 39312.4.2 Age-Related Alterations in BBB Transporter Function and Drug Response 39412.4.3 Disease-Dependent Modulation of BBB Transporters and Drug Response 39512.4.3.1 Inflammation and Pain 39512.4.3.2 Epilepsy 39612.4.4 CNS Toxicity Caused by Drug Interactions at the BBB 39812.5 Conclusions 400References 40113 Ototoxicity and Drug Transport in the Cochlea 413Stefanie Kennon-McGill and Mitchell R. McGill13.1 Auditory System Anatomy 41313.1.1 External, Middle, and Inner Ear 41313.1.1.1 Anatomy of the Inner Ear 41413.1.1.2 Hair Cell Anatomy 41413.1.2 Blood-Labyrinth Barrier 41513.2 Auditory System Physiology 41613.3 Hearing Loss, Ototoxic Drugs, and Hair Cell Damage 41613.3.1 Aminoglycosides 41713.3.2 Platinum Chemotherapeutics 41813.3.3 Salicylate 41913.4 Drug Metabolism in the Ear 41913.4.1 The Importance of Drug Metabolism in the Ear 41913.4.2 Studies of Drug-Metabolizing Enzymes in Ototoxicity 42013.4.3 Drug Transporters in the Ear 42113.5 Conclusion 423References 423Part IV Modeling Drug Metabolizing Enzymes-Transporters Interplay for The Prediction of Drug Toxicity 42714 Application of a PBPK Model Incorporating the Interplay Between Transporters and Drug-Metabolizing Enzymes for the Precise Prediction of Drug Toxicity 429Kazuya Maeda14.1 Importance of the Consideration of Intracellular Concentration of Drugs in the Tissue for Estimation of Pharmacological/Toxicological Effects of Drugs 42914.2 Extended Clearance Concept as a Tool to Explain Theoretically Transporter and Drug-Metabolizing Enzyme Interplay 43114.3 Theoretical Consideration of the Intracellular Concentration of Drugs in the Tissue 43314.4 The Benefits of Using a PBPK Model for the Accurate Prediction of Pharmacological/Toxicological Effects of Drugs 43614.5 VCT to Simulate the Distribution of Clinical Outcomes in a Specific Population with Defined Mean and Variability of Parameters in a PBPK Model 44014.5.1 VCT of Docetaxel to Estimate the Effects on the Risk of Neutropenia of Genetic Polymorphisms in OATP1B3 and MRP2 44214.5.2 VCT of Oseltamivir and Its Active Metabolite (Ro 64-0802) to Estimate the Effects on Their Brain Exposure of Genetic Polymorphisms in Multiple Uptake/Efflux Transporters 44414.5.3 VCT of Irinotecan and Its Metabolites to Estimate the Effects of Genetic Polymorphisms in Multiple Uptake/Efflux Transporters on Irinotecan-Induced Side Effects (Neutropenia, Diarrhea) 44714.6 Conclusions and Future Perspectives 450References 45115 The Extended Clearance Model: A Valuable Tool For Drug-Induced Liver Injury Risk Prediction 455Birk Poller, Felix Huth, Vlasia Kastrinou-Lampou, Gerd A. Kullak-Ublick, Michael Arand, and Gian Camenisch15.1 Introduction 45515.2 Application of the ECM to Estimate Kpuu Liver 45715.2.1 Introduction to the ECM: Concepts and Application for the Prediction of Hepatic Clearance and Drug-Drug Interactions 45715.2.2 Concept of Kpuu Liver 46015.2.3 Estimation of Kpuu Liver from In Vitro Data Using the ECM 46115.3 Relevant Concentrations for the DILI Risk Assessment 46215.3.1 Maximum Plasma Concentrations 46415.3.2 Maximum Hepatic Inlet Concentrations 46415.3.3 Maximum Intracellular Hepatocyte Concentrations 46515.4 Assessing the DIC Risk Using ECM-Based Unbound Intrahepatic Concentrations and Accounting for BSEP Inhibition as a Single Mechanism 46515.5 Assessing the DILI Risk Using the "1/R-Value Model" to Account for the Inhibition of Multiple Pathways 46715.5.1 ECM-Based 1/R-Value Model 46715.5.2 1/R vs Safety Margin Relationship 47115.6 Discussion and Outlook 473References 475Index 481
Albert P. Li, PhD, is President and CEO of In Vitro ADMET Laboratories. Dr. Li was previously Senior Fellow of Monsanto Company and Research Professor of St. Louis University Medical School. He is Chair of the Scientific Advisory Board for the Institute for Scientific Communication and the editor/co-editor of several books for Wiley, including Drug-Drug Interactions in Pharmaceutical Development (2007) and Enzyme Inhibition in Drug Discovery and Development (2009). He currently has over 180 publications in peer-reviewed journals and frequently serves as chair and speaker in national and international conferences and symposia on drug metabolism and toxicology.<
1997-2026 DolnySlask.com Agencja Internetowa
KrainaKsiazek.PL - Księgarnia Internetowa