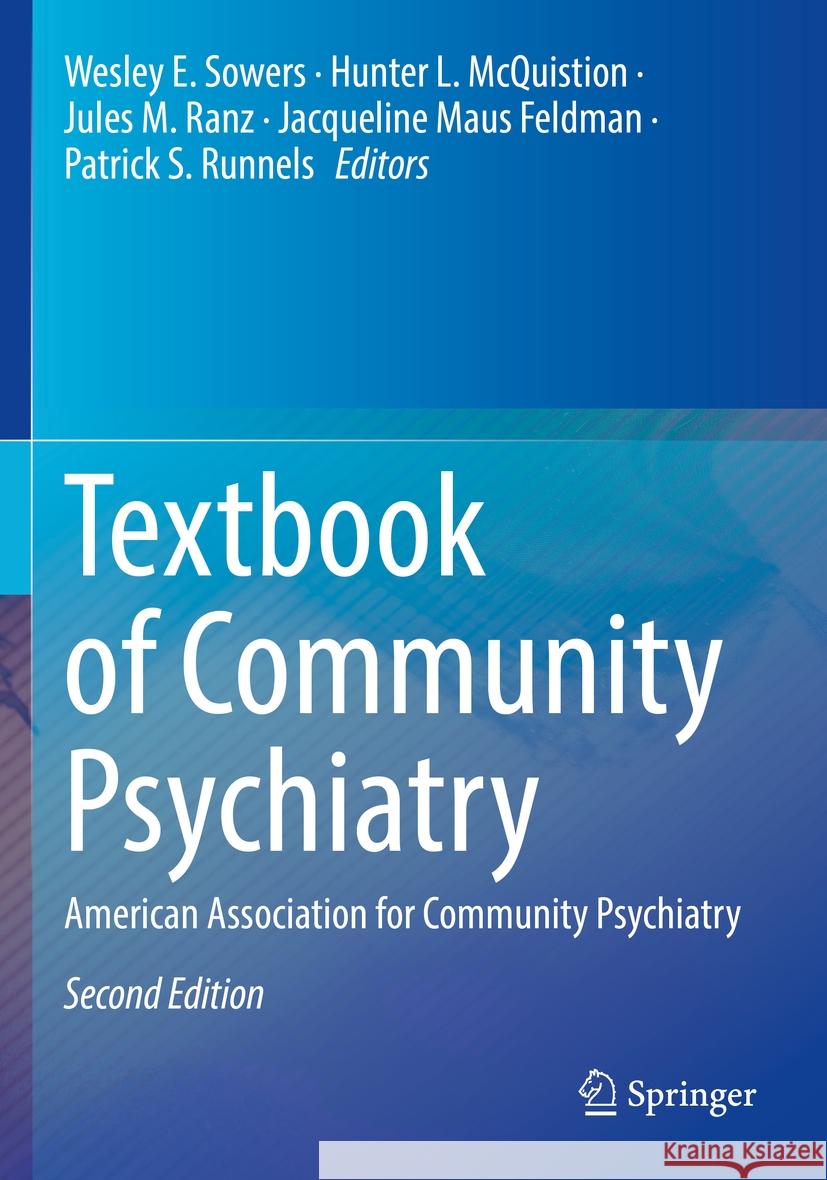
Textbook of Community Psychiatry » książka


Textbook of Community Psychiatry
ISBN-13: 9783031102417 / Angielski / Miękka / 2023
Textbook of Community Psychiatry
ISBN-13: 9783031102417 / Angielski / Miękka / 2023
(netto: 744,56 VAT: 5%)
Najniższa cena z 30 dni: 771,08 zł
ok. 20 dni roboczych.
Darmowa dostawa!
During the past decade or more, there has been a rapid evolution of mental health services and treatment technologies, shifting psychiatric epidemiology, changes in public behavioral health policy, and increased understanding in medicine regarding approaches to clinical work that focus on patient-centeredness. These contemporary issues need to be articulated in a comprehensive format. The American Association of Community Psychiatrists (AACP), a professional organization internationally recognized as holding the greatest concentration of expertise in the field, has launched a methodical process to create a competency certification in community psychiatry. As a reference for a certification examination, that effort will benefit enormously from a comprehensive handbook on the subject.
Part I Introduction and Background
1. Introduction: Community Psychiatry on the Move
2. History of Community Psychiatry
Part II The Basics: The Pillars of Community Psychiatry
3. Recovery and Person-Centered Care: Empowerment,Collaboration, and Integration
4. Population Health, Prevention, and Community Psychiatry.- Exercising Effective Leadership
5. Advocacy in Evolution: The Push and Pull of Psychiatrists
6. Comprehensive Integrated Systems of Care
Part III Core Competencies for Community Psychiatrists
7. Inspiring a Welcoming, Hopeful Culture
8. Motivational Interviewing as a Core Communication Style
9. Person-Centered Recovery Planning as a Roadmap to Recovery
10. Cultural and Linguistic Competence
11. Context-Specific Assessment
12. Team Leadership: Promoting Diversity and Inclusion in the Aftermath of COVID-19
13. Community Education
14. Collaborative Medication Management and Discontinuation
15. Traumatic Stress in the Community: Identification and Intervention
16. Integrated Care and Community Psychiatry
17. Group Appointments in Psychiatry+
18. Treatment Techniques for Co-occurring Substance
19. Use and Mental Disorders
20. Women’s Mental Health: Core Concepts for Community Psychiatry
Part IV Effective and Established Interventions
21. Developing, Evaluating and Implementing Evidence-Based Interventions in Real World Practice
22. Cognitive Behavioral Therapy
23. Psychiatric Rehabilitation
24. Family Systems Care in Public Sector Settings
25. Evidence-Based Practices for Co-occurring Addiction and Mental Illness
26. Case Management and Assertive Community Treatment
27. Crisis and Emergency Services
Part V Creating Healthy Communities
28. Epidemiology in Community Psychiatry
29. Social and Political Determinants of Health and Mental Health
30. Mental Health Services Research and Community Psychiatry
31. Climate Change: Implications for Community Mental Health
32. Disaster Victims and the Response to Trauma
33. The Role of the Psychiatrist in Community Consultation and Collaboration
34. Collaborative Reduction of Criminal Justice Involvement for Persons with Mental Illness
Part VI Supportive Services for Community Living
35. Housing First and the Role of Psychiatry in Supported Housing
36. Health Self-Management: The Emerging Importance of Trauma and Resilience
37. Supported Employment.- Peer Service Providers as Colleagues
38. Fountain House and the Clubhouse Movement
40. Service Coordination and Health Homes
Part VII Special Populations
41. Community-Based Psychiatric Care for Individuals with Intellectual and Developmental Disabilities
42. Psychiatric Care for People Experiencing Homelessness
43. Early Psychosis and the Prevention and Mitigation of Serious Mental Illness
44. Cognitive Behavior Therapy for Psychosis
45. Veterans’ Services
46. Child and Adolescent Psychiatric Services
47. Serving Elders in the Public Sector
48. Rural Populations
49. Clinical Issues and Programming for Sexual and Gender Minority Populations
50. Migrant and Refugee Mental Health
Part VIII Development and Administration of Services
51. Transforming Mental Health Systems and Programs
52. Program Evaluation
53. Creating Value: Resource and Quality Management
54. Telehealth and Technology
55. The Medical Director in Community-Based Mental Healthcare
56. Financing of Community Behavioral Health Services
57. Workforce Development in Community Psychiatry
58. Practical Ethics for Practicing Clinicians
Part IX Shaping the Future
59. Medical Student and Resident Education in Community Psychiatry
60. Public/Community Psychiatry Fellowships
61. Mentoring and Supervision in Community Psychiatry
62. International Trends in Community Mental Health Services
63. Community Psychiatry: Past, Present, and Future.
Wesley E. Sowers, MD is Clinical Professor of Psychiatry at the University of Pittsburgh Medical Center and is the Director of the Center for Public Service Psychiatry and its associated Fellowship Program at Western Psychiatric Hospital. He is board certified in Adult Psychiatry with subspecialty certifications in Addiction, Administrative and Community Psychiatry. He is a Past President of the American Association for Community Psychiatry and has served on the Board of Directors of that organization since 1988. He has also been on the Board of the American Association of Psychiatric Administrators since 1999. He has served as Co-Chair of the Mental Health Services Committee of the Group for Advancement of Psychiatry since 2009. From 2008 to 2016 he was co-director of the SAMHSA sponsored Recovery to Practice curriculum development project for psychiatry.
Dr. Sowers is a graduate of Brown University and Northwestern University Medical School. He completed residencies at the Cook County Hospital in Chicago and the Albert Einstein College of Medicine, Department of Psychiatry in New York City. Clinically, he has extensive experience in the provision of treatment and services to special populations such as homeless men and women, people with criminal records, LGBTQ individuals, and people with substance use disorders. He has published several articles, editorials, and book chapters on topics related to his clinical activities and health care systems management. He was the chief architect of the Level of Care Utilization System (LOCUS) and its counterpart for children and adolescents (CALOCUS), instruments widely used to guide service intensity decisions.Hunter L. McQuistion, MD is Clinical Professor of Psychiatry at New York University (NYU) Grossman School of Medicine and Senior Attending Psychiatrist at NYU Langone Health. He is Medical Director of the SAMHSA-funded Engagement, Treatment, and Recovery (EnTRy) Program at Family Health Centers at NYU Langone, which provides FQHC-based multidisciplinary and recovery-oriented services to underserved Brooklyn residents experiencing serious mental health challenges. He recently completed a successful and satisfying stewardship as Chief of Psychiatry & Behavioral Health at NYC Health+Hospitals|Gotham|Gouverneur. Among other roles in systems management and clinical policy, Dr. McQuistion has also served at a high level in the City of New York Department of Health & Mental Hygiene.
As an academic community psychiatrist, he has focused much of his career on program development and scholarship concerning people who experience homelessness and mental illnesses, but has also turned energies to other underserved populations, including interest in efforts on racial and ethnic issues as related to clinical competencies. Spanning roles in advocacy, administration, epidemiological and services research, and education, Dr. McQuistion has published and presented widely. He offers program and educational consultation as well as providing direct clinical services. Among other accomplishments, Dr. McQuistion is a Past President of the American Association for Community Psychiatry, is recognized as an Exemplary Psychiatrist by the National Alliance on Mental Illness, is a Distinguished Life Fellow of the American Psychiatric Association, a Fellow of the New York Academy of Medicine, and a member of the Group for Advancement of Psychiatry.
Jules M. Ranz, MD is Clinical Professor of Psychiatry at Columbia. He was director of the Public Psychiatry Fellowship at NYS Psychiatric Institute/Columbia University Medical Center from 1992 to 2017 and continues as a mentor to many of the over 300 psychiatrists who completed the fellowship. The Public Psychiatry Fellowship is generally acknowledged to be the premier program of its kind in the country, supported by three published surveys of its alumni. In the past fifteen years, over twenty other public/community psychiatry fellowships have been created, many modeled on the Columbia program as described in “Core Elements of a Public Psychiatry Fellowship” published in 2008. During this time Dr. Ranz has created a network of directors of these programs that led to the publication of five articles about that network, as well as six articles about individual fellowships in that network.
Dr. Ranz was principal author of a 2006 published article written by the Mental Health Services Committee of the Group for the Advancement of Psychiatry, utilizing data to demonstrate that early and mid-career psychiatrists spend more time in publicly-funded organizational settings than in solo office practice. A follow up paper described a 12 site study conducted by Dr. Ranz and that same committee: "A Four Factor Model of Systems- Based Practices in Psychiatry" published in 2012. In recognition of his long career as a public psychiatry educator, Dr. Ranz received the 2013 APA/NIMH Vestermark Psychiatry Educator Award. Following his semiretirement from the Columbia Fellowship, Dr. Ranz helped to create a Community Psychiatry Nurse Practitioner fellowship at a Federally Qualified Health Center, which was described in a 2021 publication in Psychiatric Services. He is continuing to serve as an advocate for bringing psychiatric nurse practitioners and psychiatrists together to collaborate on organizational, academic and advocacy strategies.
Jacqueline Maus Feldman, MD is a Professor Emerita with the School of Medicine, Department of Psychiatry and Behavioral Neurobiology at the University of Alabama at Birmingham (UAB). She retired in July 2014, as the Patrick H. Linton Professor, the Medical Director of the UAB Community Psychiatry Program, the Executive Director of the UAB Comprehensive Community Mental Health Center, the Director of the Division of Public Psychiatry, and the Vice Chair for Clinical Affairs. She continues to provide clinical and administrative services for the department, has consulted with Alabama Medicaid, and serves as the National Alliance on Mental Illness (NAMI) national Associate Medical Director. She has also served as the federal court monitor for women’s mental health in the Alabama Department of Corrections and participated with the Department of Justice in its investigation of Georgia State Hospitals. She has also served on numerous national and regional planning and review committees, is a Past-President of the Alabama Psychiatric Physicians Association, Past President of the American Association for Community Psychiatry and has served on the Board of the American Psychiatric Foundation, as well as the Alabama NAMI Board. She has served on the American Psychiatric Association Annual Meeting Scientific Program Committee as member and Chair. Her areas of research included effectiveness of ACT, dual diagnosis, jail diversion, and treatment of perinatal depression. She has published and spoken extensively on affective disorders, schizophrenia, dual diagnosis, public policy development, advocacy, mental health and criminal justice, and recovery, and is the immediate past Editor-In-Chief of the Community Mental Health Journal.
Dr. Feldman has been listed numerous times in “Best Doctors in America” and named by NAMI three times as an Exemplary Psychiatrist.
Patrick S. Runnels, MD, MBA serves as both Chief Medical Officer of Population Health and Vice Chair of Psychiatry for University Hospitals in Cleveland. Additionally, he holds an academic appointment as Professor at the Case Western Reserve University School of Medicine, where he founded the Public and Community Psychiatry Fellowship. He was the founding chair and remains an active member The National Council on Mental Wellness Medical Director Institute. He has served in the past on the Board of Trustees for the American Psychiatric Association, The National Alliance on Mental Illness (Ohio Chapter), and the American Association for Community Psychiatry. He has also served as Chair of the Council on Advocacy and Government Relations for the American Psychiatric Association. Dr. Runnels received his medical degree from the University of Missouri, Columbia; had his psychiatric residency at the Mount Sinai Hospital in New York City, then completed the Columbia University’s Fellowship in Public Psychiatry. He received his Executive MBA at Case Western Reserve University Weatherhead School of Management. He has published several articles, editorials, and book chapters, as well as given numerous national talks and presentations in the areas of healthcare leadership and clinical transformation.
The second edition of the AACP's (American Association for Community Psychiatry) Textbook of Community Psychiatry is a welcome update of this notable work that comprehensively presents the state of the art in this field. Along with continuously evolving scientific advances and principles of clinical care, community psychiatry must respond to shifts in public policy as well as economic climate. The past decade has witnessed significant political and social changes, including climate change, immigration levels, technological advancement, the influence of social media and the rise of political unrest. This new edition reflects these wider changes, incorporating new chapters and enhancing previous ones. It remains the standard text for certification of those working in healthcare and social welfare systems design and delivery of services.
Readers will gain knowledge of:
- Basic pillars of the field
- Evidence based interventions
- Telepsychiatry and technological aids
- Trauma informed services
- Integrated health systems
- Social determinants of health
- Structural discrimination
1997-2024 DolnySlask.com Agencja Internetowa
KrainaKsiazek.PL - Księgarnia Internetowa