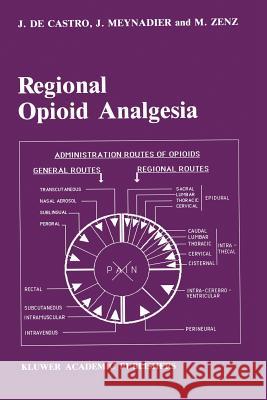
Regional Opioid Analgesia: Physiopharmacological Basis, Drugs, Equipment and Clinical Application » książka


Regional Opioid Analgesia: Physiopharmacological Basis, Drugs, Equipment and Clinical Application
ISBN-13: 9789401075435 / Angielski / Miękka / 2012 / 640 str.
Regional Opioid Analgesia: Physiopharmacological Basis, Drugs, Equipment and Clinical Application
ISBN-13: 9789401075435 / Angielski / Miękka / 2012 / 640 str.
(netto: 1150,16 VAT: 5%)
Najniższa cena z 30 dni: 1156,64
ok. 16-18 dni roboczych.
Darmowa dostawa!
by E.K. ZSIGMOND, M.D. Department of Anesthesiology University of Illinois Chicago U.S.A. It is, indeed, a distinct honor and privilege to be invited by the authors to write a preface to this monumental monograph, Regional Opioid Analgesia. Regional Opioid Analgesia is a colossal undertaking by Drs. De Castro, Meynadier and Zenz shortly after the introduction of this revolutionary approach to pain relief which opened a new epoch in analgesiology. This is, indeed, the first authentic and comprehensive textbook encompassing the current knowl- edge on this novel approach to pain relief. We are indebted to the authors for introducing the new opioids to regional analgesia with the scientists, who de- veloped the potent short and ultrashort acting opioids with high therapeutic indices, which many researchers dreamt about but never before materialized. The side effect liabilities of these new opioids are minute as compared to morphine and meperidine. Regional Opioid Analgesia could not have been more authentically written than by Drs. De Castro,Zenz and Meynadier,who have conducted daily clinical investigations on all known opioids for regional analgesia as well as for neurolept analgesia. Therein lies the great value of this monograph: it is the most authentic work on this topic.
I: Anatomical, Pharmacological, Physiological and Technical Basis of Spinal Regional Opioid Administration.- 1. Developments, advantages and drawbacks of regional opioid analgesia.- 2. Anatomy and physiology.- 2.1 Nociception and nociceptive pathways.- 2.2 Anatomy of opioid receptors.- 2.3 Anatomy of the epidural and the intrathecal spinal space.- 3. Micropharmacology of antinociceptive substances in the spinal cord.- 3.1 Endorphins.- 3.2 Multiple opioid receptors.- 3.3 Opioid agonists, opioid antagonists.- 3.3.1 Agonists.- 3.3.2 Antagonists.- 3.3.2.1 Pure antagonists.- 3.3.2.2 Mixed agonist-antagonists.- 3.3.2.3 Partial agonist-antagonists.- 3.4 Endogenous non-opioid neuropeptides and neuroamines.- 3.4.1 Substance P.- 3.4.2 Other peptides and amines.- 3.5 Other exogenous substances with spinal antinociceptive action.- 4. Pharmacokinetics of opioids.- 4.1 Molecular weight [dalton].- 4.2 Lipid solubility, hydrosolubility.- 4.3 Ionization.- 4.4 Protein binding.- 4.5 Distribution volume.- 4.6 Plasma half life times.- 4.7 Clearance.- 4.8 Permeability across biological membranes.- 4.9 Diffusion of spinal opioids.- 4.10 Specific receptor binding activity.- 4.11 Rediffusion.- 4.12 Physical characteristics of opioid solutions.- 4.12.1 Volume, density, specific gravity, baricity.- 4.12 2 Changes in body temperature.- 4.12.3 Changes in intraspinal pressure.- 4.13 Special pharmacokinetics of spinal opioids.- 4.14 Pharmacokinetic variability.- 5. Pharmacodynamics of opioids.- 5.1 Analgesia.- 5.1.1 Relationship between administration route and dose.- 5.1.2 Relationship between dose and depth of analgesia.- 5.1.3 Relationship between dose and duration of analgesia.- 5.1.4 Relationship between lipid soluble substances and duration of analgesia.- 5.1.5 Relationship between analgesia and pain aetiology.- 5.2 Cardiovascular system and sympathetic nervous system.- 5.3 Respiratory system.- 5.4 Muscular system and gastrointestinal system.- 5.5 Central nervous system.- 5.6 Endocrine and metabolic system.- 6. Side effects.- 6.1 Generalities.- 6.2 Side effects of epidural opioids.- 6.2.1 Early and delayed respiratory depression.- 6.2.1.1 Aetiology and characteristics.- 6.2.1.2 Monitoring.- 6.2.1.3 Factors increasing or reducing the risk of delayed respiratory depression.- 6.2.1.4 Dose response curves.- 6.2.1.5 Prophylaxis.- 6.2.1.6 Treatment.- 6.2.2 Pruritus.- 6.2.3 Nausea and vomiting.- 6.2.4 Urinary retention.- 6.2.5 Constipation.- 6.2.6 Drowsiness.- 6.2.7 Other rarer side effects.- 6.2.8 Overdose, addiction, dependence, tolerance and withdrawal syndrome.- 6.3 Side effects of intrathecal opioids.- 6.3.1 Respiratory depression.- 6.3.2 Other side effects.- 6.3.3 Prevention of side effects after intrathecal administration.- 6.4 Tolerance, tachyphylaxis.- 6.4.1 Definition and characteristics.- 6.4.2 Rapidity of appearance.- 6.4.3 Reversibility of tolerance.- 6.4.4 Cross tolerance.- 6.4.5 Methods of delaying tolerance development.- 6.5 Side effects due to the technique used.- 6.5.1 Fibrotic reactions.- 6.5.2 Neuronal degeneration.- 6.5.3 Infection.- 6.5.4 Virus reactivation.- 7. Drugs.- 7.1 Pure opioid agonists.- 7.1.1 Morphine.- 7.1.2 Diamorphine (heroin).- 7.1.3 Pethidine (meperidine).- 7.1.4 Methadone.- 7.1.5 Hydromorphone.- 7.1.6 Nicomorphine.- 7.1.7 Fentanyl.- 7.1.8 Alfentanil.- 7.1.9 Sufentanil.- 7.1.10 Lofentanil.- 7.1.11 DADL.- 7.1.12 Metenkephalin.- 7.1.13 Beta-endorphin.- 7.1.14 Spiradoline 5 UI-62, 0066E.- 7.2 Mixed opioid agonist-antagonists and partial agonist-antagonists.- 7.2.1 Buprenorphine.- 7.2.2 Nalbuphine.- 7.2.3 Butorphanol.- 7.2.4 Pentazocine.- 7.2.5 Meptazinol.- 7.2.6 Tramadol.- 7.3 Pure opioid antagonists.- 7.3.1 Naloxone.- 7.3.2 Nalmefene.- 7.3.3 Naltrexone.- 7.4 Non-opioid drugs.- 7.4.1 Calcitonin.- 7.4.2 Droperidol.- 7.4.3 Baclofen.- 7.4.4 Midazolam.- 7.4.5 Ketamine.- 7.4.6 Clonidine.- 7.4.7 Lysine-acetylsalicylate.- 7.4.8 Somatostatin.- 7.4.9 Enkephalinase and aminopeptidase inhibitors.- 7.4.10 Cholecystokinin inhibitors: proglumide or xylamide.- 7.5 Adrenaline (Epinephrine).- 7.6 Drug-related problems.- 7.6.1 Physical properties.- 7.6.1.1 Solutions.- 7.6.1.2 Stereospecificity.- 7.6.1.3 pH.- 7.6.2 Preservative-free products.- 7.6.3 Doses.- 7.6.4 Drug interactions.- 7.6.5 Drug associations.- 7.6.5.1 Local anaesthetics.- 7.6.5.2 Other drug associations.- 7.6.6 Drug administration modalities.- 7.6.6.1 Patient’s position.- 7.6.6.2 Injection volumes.- 7.6.6.3 Level of administration.- 7.6.6.4 Injection routes.- 8. Equipment and drug delivery systems.- 8.1 Equipment.- 8.1.1 Epidural, intrathecal needles.- 8.1.2 Catheters.- 8.1.2.1 Materials and models.- 8.1.2.2 Catheter problems.- 8.1.2.3 Externalized or tunnelled catheter.- 8.1.2.4 Open or closed systems.- 8.1.3 Micropore filters.- 8.2 Drug delivery systems.- 8.2.1 Ports.- 8.2.2 Special drug delivery systems.- 8.2.2.1 Roquefeuil’s self-administration system.- 8.2.2.2 Muller and Laugner’s self-administration device.- 8.2.2.3 Self-administration device Secor.- 8.2.3 Pumps.- 8.2.3.1 Pros and cons of pump devices.- 8.2.3.2 External pumps.- 8.2.3.3 Implantable pumps.- 8.2.4 Dressings.- 8.2.4.1 Transparent dressing.- 8.2.4.2 Cross elastic wound dressing.- 8.2.4.3 Unguent.- 83 Drug administration techniques.- 8.3.1 Single shot technique.- 8.3.1.1 Epidural.- 8.3.1.2 Intrathecal.- 8.3.2 Catheter placement.- 8.3.3 Percutaneous catheter fixation.- 8.3.4 Subcutaneous tunneling.- 8.3.5 Port implantation.- 8.3.6 Pump implantation.- 8.3.6.1 Implantation technique for the Infusaid ® pump.- 8.3.6.2 Implantation technique for the Synchromed ® pump.- 8.3.7 Intracerebroventricular port implantation.- 8.3.8 Injection into a port, refill of a pump.- 8.3.9 Injection-infusion techniques.- 8.3.10 Pros and cons of continuous infusion.- 8.3.10.1 Advantages.- 8.3.10.2 Drawbacks.- 8.3.10.3 Drug selection for continuous infusion.- 8.4 Nursing.- 8.4.1 Catheter problems.- 8.4.2 Port problems.- 8.4.3 Pump problems.- II: Clinical Practice of Spinal Opioid Administration.- 9. Clinical applications, generalities.- 10. Intraoperative use.- 10.1 Epidural administration.- 10.1.1 Opioids in association with general anaesthesia.- 10.1.2 Epidural somatostatin.- 10.1.3. Epidural opioids in association with local anaesthetics.- 10.2 Intrathecal administration.- 10.2.1 Intrathecal morphine in association with thiopentone anaesthesia.- 10.2.2 Intrathecal pethidine for spinal anaesthesia in high doses (1 mg/kg).- 10.2.3 Intrathecal association of opioids with local anaesthetics.- 10.2.4 Intrathecal association of an opioid and clonidine.- 10.3 Particular problem: extracorporeal shock wave lithotripsy.- 11. Postoperative pain.- 11.1 Potential advantages and drawbacks.- 11.1.1 Better pain relief?.- 11.1.2 Improved pulmonary function?.- 11.1.3 Reduced side effects?.- 11.1.4 Better in selected groups of patients?.- 11.1.5 Superior to other analgesia methods?.- 11.1.6 Better clinical outcome?.- 11.2 Selection of patients.- 11.2.1 Spinal opioids in children.- 11.3 Selection of drugs and routes of administration.- 11.3.1 Morphine and methadone.- 11.3.2 Epidural lipophilic opioids.- 11.3.3 Associations of opioid and local anaesthetic.- 11.3.4 Non-opioid products.- 11.4 Selection of injection technique.- 11.4.1 Repeated bolus injection and patient controlled analgesia (PCA).- 11.4.2 Continuous infusion.- 11.4.3 Continuous plus on demand infusion.- 11.5 Selection of equipment: pumps and ports.- 11.6 Precautions and surveillance.- 11.7 Side effects.- 11.8 Indications and contra-indications for postoperative epidural opioid analgesia.- 11.9 Nursing.- 12. Other applications in acute pain situations.- 12.1 Posttraumatic pain.- 12.2 Intensive care unit patients.- 12.3 Myocardial infarction.- 12.4 Visceral pain after arterial embolisation.- 12.5 Acute pancreatitis.- 12.6 Headache following dural puncture.- 12.7 Diagnosis of pain aetiology.- 13. Obstetrics.- 13.1 Potential advantages, drawbacks and indications.- 13.1.1 Justification of better analgesia.- 13.1.2 Potential advantages.- 13.1.3 Potential disadvantages.- 13.1.4 Potential indications.- 13.2 Labour and delivery pain.- 13.2.1 Epidural opioids.- 13.2.1.1 Morphine.- 13.2.1.2 Pethidine.- 13.2.1.3 Fentanyl.- 13.2.1.4 Morphine + bupivacaine.- 13.2.1.5 Lipophilic opioid + local anaesthetic.- 13.2.2 Intrathecal opioids.- 13.2.2.1 Morphine.- 13.2.2.2 Beta-endorphin.- 13.2.2.3 Fentanyl + bupivacaine.- 13.2.2.4 Naloxone infusion for reduction of side effects.- 13.2.2.5 Naltrexone orally for reduction of side effects.- 13.2.3 Global evaluation.- 13.3 Postcaesarean section.- 13.3.1 Epidural opioids.- 13.3.1.1 Morphine.- 13.3.1.2 Methadone.- 13.3.1.3 Hydromorphone.- 13.3.1.4 Pethidine.- 13.3.1.5 Fentanyl.- 13.3.1.6 Sufentanil.- 13.3.1.7 Butorphanol.- 13.3.1.8 Meptazinol.- 13.3.1.9 Buprenorphine.- 13.3.1.10 Opioids associated with local anaesthetics.- 13.3.2 Intrathecal opioids.- 13.4 Side effects of spinal opioids in obstetrics.- 13.4.1 Maternal side effects.- 13.4.2 Foetal side effects.- 13.5 Post-partum episiotomy.- 13.6 Prostaglandin abortion.- 13.7 Pre-eclampsia.- 13.8 Precautions and surveillance.- 13.9 Survey of the principal clinical reports.- 14. Cancer pain.- 14.1 Analgesic ladder.- 14.2 Potential advantages.- 14.3 Selection of patients.- 14.4 Selection of drugs.- 14.4.1 Opioids.- 14.4.2 Associations of an opioid and a local anaesthetic.- 14.4.3 Associations of an opioid and another product.- 14.5 Administration modalities.- 14.5.1 Injection route: epidural or intrathecal?.- 14.5.2 Intrathecal isobaric or hyperbaric solution?.- 14.5.3 Repeated bolus or continuous plus on-demand infusion?.- 14.5.3.1 Percutaneous epidural catheter for bolus injection.- 14.5.3.2 Tunnelled epidural catheter.- 14.5.3.3 Tunnelled intrathecal catheter.- 14.5.3.4 External unidirectional valves.- 14.5.3.5 Implanted ports.- 14.5.4 Continuous plus on-demand infusion with pumps and ports.- 14.5.4.1 Portable infusion pump.- 14.5.4.2 Implanted infusion pump with epidural catheter.- 14.5.4.3 Implanted infusion pump with intrathecal catheter.- 14.6 Potential drawbacks of spinal opioid drugs.- 14.6.1 Side effects.- 14.6.2 Technical problems.- 14.6.2.1 Pain on epidural injection.- 14.6.2.2 Fibrous mass.- 14.6.2.3 Infection.- 14.6.2.4 Catheter dislodgement or occlusion.- 14.6.2.5 Port failure.- 14.6.2.6 Pump failure.- 14.6.3 Dose escalation and tolerance.- 14.7 Multicenter survey.- 14.7.1 Epidural administration.- 14.7.2 Intrathecal administration.- 14.8 Intracisternal opioids.- 14.9 Intracerebroventricular opioids.- 14.9.1 Indications and contra-indications.- 14.9.2 Technique.- 14.9.3 Effects.- 14.9.4 Reinjection and daily nursing.- 14.9.5 Side effects and complications.- 14.9.6 Results.- 14.10 Current care and nursing problems during regional opioid analgesia.- 15. Chronic non-malignant pain.- 15.1 Treatment with epidural opioids.- 15.2 Treatment with intrathecal opioids and/or non-opioid drugs.- 16. Perineural opioid analgesia (PNOA).- 17. Comparative evaluation of the risk/benefit ratio.- 17.1 Epidural opioid analgesia versus peroral, intravenous or intramuscular opioids.- 17.2 Epidural opioids versus intravenous patient controlled analgesia.- 17.3 Epidural opioids versus epidural anaesthesia with a local anaesthetic.- 17.4 Epidural opioid versus intrathecal opioid.- 17.5 Advantages and drawbacks of intrathecal opioid analgesia.- 17.6 Limits and contra-indications of regional opioid analgesia.- 18. Future directions in spinal opioid research and conclusions.- 19. What is regional opioid analgesia?.- 20. Technical data of equipment for spinal opioid therapy.- 20.1 Special needles.- 20.2 Epidural or intrathecal catheters.- 20.3 Filters.- 20.4 Extension tube for connection between pumps and ports and catheters.- 20.5 Implantable catheter access port.- 20.6 Infusion pumps.- 20.7 Monitoring devices.- Bibliography and references.- Addendum to the Bibliography and references.- Index of subjects.
Michael Zenz wurde 1986 zum apl. Professor der Medizinischen Hochschule Hannover ernannt. Im selben Jahr folgte er einem Ruf der Ruhr-Universität Bochum, wurde Direktor der Universitätsklinik für Anästhesiologie, Intensiv- und Schmerztherapie am Bergmannsheil und 2001 zusätzlich Direktor an der Universitätsklinik Knappschaftskrankenhaus Bochum-Langendreer. Professor Zenz ist Präsident der Deutschen Gesellschaft zum Studium des Schmerzes (DGSS), Ehrenmitglied der Sertürner-Gesellschaft, Sprecher des Arbeitskreises Schmerztherapie der Deutschen Gesellschaft für Anästhesiologie und Intensivmedizin (DGAI), Mitglied zahlreicher wissenschaftlicher Gesellschaften sowie Herausgeber internationaler wissenschaftlicher Zeitschriften.
1997-2026 DolnySlask.com Agencja Internetowa
KrainaKsiazek.PL - Księgarnia Internetowa